Edgar Pérez-Barragán1, María Fernanda Cid-Ramírez 2, José Humberto Castillo-Flores3, Enver Augusto Velasco-Cuevas4, Samantha Pérez-Cavazos 5
1 Infectious Diseases Department, Hospital de Infectología, Centro Médico Nacional La Raza, México City, México. edgar.pbarragan@gmail.com ORCID ID: 0000-0002-3839-1567
2 Facultad de Medicina. Universidad Anáhuac de Puebla. San Andrés Cholula, Puebla, México. fernanda027cidr@gmail.com ORCID ID: 0000-0002-3123-8877
3 Department of Hospital Epidemiology and Infection Prevention, Hospital Christus-Muguerza Betania, Puebla, Mexico. CP 72501. jhcastillo.fl@gmail.com ORCID ID: 0000-0003-3190-8778
4 Department of Child and Adult Medicine for Rural Health Services, Centro de Ayuda CORBAN A.C. Villa de Tututepec de Melchor Ocampo, Oaxaca, México. CP 71830. enver_99@hotmail.com ORCID ID: 0000-0001-9953-4376
5 Department of Hospital Epidemiology and Infection Prevention, Hospital Christus-Muguerza Betania, Puebla, Mexico. CP 72501. samanthaperezc@gmail.com ORCID ID: 0000-0002-1222-1930
Running head: Tuberculous mastitis
Conflict of interest: All authors report no conflicts of interest with this article.
Corresponding and reprints: Samantha Pérez Cavazos, MD
Department of Hospital Epidemiology and Infection Prevention, Hospital Christus-Muguerza Betania, Puebla, Mexico.
CP 72501
Contact: (81) 10-17-64-77, e-mail: samanthaperezc@gmail.com
Abstract
Background: Breast tuberculosis is a rare and non-malignant form of inflammation characterized by distinct histological lesions that show fibrosis, eosinophils, and necrosis, distinguishing it from other types of granulomatous mastitis. Tuberculous mastitis (TBM) is another term used to describe this condition, which represents less than 0.1% of all breast diseases and less than 2% of all tuberculosis cases.
Case presentation: In August 2021, a 33-year-old pregnant woman from Mexico discovered a nodular lesion in her left breast that progressively grew in size. Following evaluation, she received a diagnosis of chronic granulomatous mastitis with abscess and focal sclerosing adenosis based on a biopsy of the lesion. Special histochemical stains such as Periodic Acid-Schiff, Gram, and Ziehl-Neelsen were conducted, revealing the presence of Acid-Fast Bacilli. As a result, anti-tuberculous therapy was initiated in December 2021.
Conclusions: Breast tuberculosis is a rare manifestation of tuberculosis that can mimic malignant breast lesions. It is essential to differentiate it accurately to ensure prompt initiation of appropriate treatment.
Keywords: Tuberculosis, breast tuberculosis, Mycobacterium tuberculosis, tuberculous mastitis.
Introduction
Mycobacterium tuberculosis is the causative agent of tuberculosis (TB), a disease that can affect various organs in the body, with the lungs being the most commonly affected site. However, around 15% of TB cases manifest solely as extrapulmonary disease. Granulomatous mastitis is characterized by the development of a painful lump in the breast. Inflammation may also result in swelling and redness of the affected breast. Other symptoms can include changes in the nipple and areola, such as retraction, fistula, or ulceration. A significant proportion of patients, approximately 37%, may present with signs of an abscess (1, 2).
BT is a rare condition that constitutes less than 0.1% of all breast pathologies observed histologically (1).
CASE REPORT
A 33-year-old pregnant woman from Oaxaca, Mexico, who has a history of Diabetes Mellitus type 2 and no significant family history of cancer, presented with a nodular lesion in her left breast. Her gynecological history revealed that she was in her third pregnancy, with one previous successful birth and one previous abortion.
The patient initially noticed a painless palpable lump in the lower left quadrant of her left breast during the early weeks of her pregnancy. She discovered it through breast self-examination. Over a period of three months, the lump increased in size, and she developed a purulent nipple discharge. However, she did not experience fever or abnormal blood pressure. A breast ultrasound was performed, revealing a complex lesion in the left breast classified as BIRADS-3. The lesion was identified as granulomatous mastitis located at the 5 o’clock radius, 35mm away from the nipple. It measured 22.3 x 25.0 x 15.0 mm with irregular and partially defined borders, hypoechoic content, an acoustic shadow at the posterior level, and no central vascularity on color Doppler application. A biopsy of the lesion confirmed the diagnosis of chronic granulomatous mastitis with abscess and focal sclerosing adenosis. Additional histochemical staining with Periodic Acid-Schiff (PAS), Gram, and Ziehl-Neelsen stains revealed the presence of acid-fast bacilli, leading to a diagnosis of tuberculous mastitis at 18 weeks of pregnancy. Figure 1.
She was treated with oral anti-tuberculosis therapy consisting of isoniazid (75mg), rifampicin (150mg), pyrazinamide (400mg), and ethambutol (300mg) for the first two months, followed by isoniazid and rifampicin for the remaining four months. This treatment regimen is standard in Mexico for tuberculosis.
At 28 weeks of gestation, a fetal ultrasound showed a small-for-age fetus and decreased placental flow. The patient received continued anti-tuberculosis treatment and enoxaparin to improve placental oxygen bioavailability. At 36.4 weeks gestation, a follow-up obstetric ultrasound revealed a healthy single fetus with appropriate weight for gestational age, and normal Doppler flucometry readings of the umbilical, middle cerebral, and uterine arteries. The pregnancy was successfully resolved through cesarean section without maternal and fetal complications. The patient’s clinical symptoms resolved completely with oral TB treatment.
Discussion
Tuberculous mastitis is an extremely rare form of breast disease, accounting for less than 0.1% of all breast pathologies and less than 2% of all cases of tuberculosis (3). This condition typically affects young, lactating women who have had multiple pregnancies and are between the ages of 20 and 40, as in the present patient (4).
The National Tuberculosis Program of the Mexican Ministry of Health reported 20,285 new TB cases in 2019, with 80% of cases being pulmonary tuberculosis. In Mexico, the incidence of this pathology in general in 2022 ranged from 19-32 cases per 100,000 inhabitants (5).
Pregnant women with comorbidities, such as diabetes, are at an increased risk for developing extrapulmonary tuberculosis (EPTB). EPTB is becoming more common, particularly in individuals with HIV co-infection or other immunocompromising conditions.
In a small percentage of cases (3-30%), the manifestation is bilateral and multiple lesions are rarely seen. Symptoms such as nipple and skin retractions and axillary lymphadenopathies can also be observed, which can simulate carcinoma (4). There are three categories in the classification of tuberculous mastitis: nodular, disseminated, and abscess varieties. In the patient’s case, the lesion exhibited characteristics of all three categories (6).
Mammography may show breast mass and skin thickening, but these findings are non-specific, with about 50% of cases reported as BIRADS 4/5. Ultrasound can be helpful in evaluating the relationship between the lesion and the chest wall (7). In the case of the patient, the ultrasound showed a granulomatous lesion and inflammation of lymph nodes. (4).
From a histopathological perspective, breast tuberculosis needs to be distinguished from other granulomatous processes, including Mycobacterium avium complex (in immunocompromised patients), sarcoidosis, bartonellosis, granulomatous reactions in breast cancer, duct ectasia, acute mastitis, granulomatosis with polyangiitis, and infections caused by Taenia solium, Salmonella typhi, and Histoplasma capsulatum. Therefore, a thorough differential diagnosis is crucial to ensure accurate diagnosis and effective treatment (8).
In order to detect acid-fast bacilli (AFB) in a smear, there must be more than 10,000 organisms/mL, and the Ziehl-Neelsen staining method is considered the gold standard for identifying the growing tuberculosis bacilli. Nucleic acid amplification tests (NAAT) and polymerase chain reaction (PCR) can provide rapid and specific diagnoses of TB, but have lower sensitivity, particularly in cases where AFB smear results are negative (9).
In the case of the woman discussed, a breast biopsy was performed, and Ziehl-Neelsen staining of the sample was positive for AFB.
The recommended therapy is 6 months of antituberculous treatment. In this case, the patient was started on 6 months of antituberculous therapy, with the possibility of extending it to 1 year if necessary.
Tuberculosis in pregnancy is an important factor in maternal mortality, and if left untreated, it poses a definite risk for transmission of the disease to the newborn. While isoniazid, rifampicin, and ethambutol are all classified as Food Drug Administration (FDA) pregnancy category C, there is available data that does not suggest any significant adverse maternal-fetal effects (10).
Breast tuberculosis is a rare form of tuberculosis that may be mistaken for malignant breast lesions, highlighting the importance of an accurate diagnosis and prompt treatment. It is crucial to consider the risk factors associated with this condition to facilitate early detection and management.
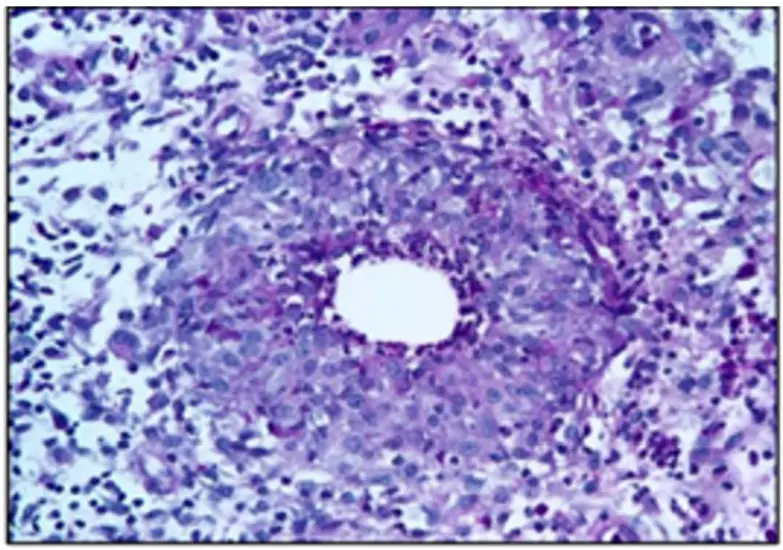
PAS staining highlights the granuloma macrophages.
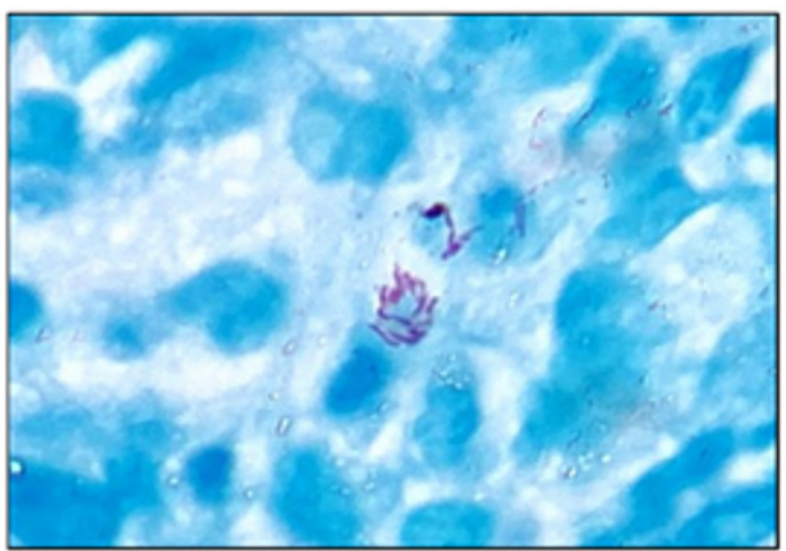
ZN staining demonstrates bacillary structures of intense eosinophilic color.
List of abbreviations
TB – Tuberculosis
EPTB – Extrapulmonary tuberculosis
PAS – Periodic acid–Schiff
TBM- Tuberculous mastitis
CT-Computed tomography scan
MRI-Magnetic resonance imaging
AFB- Acid-Fast Bacilli
PCR-Polymerase chain reaction
FDA-Food Drug Administration
FNA-Fine needle aspiration
BT-Breast tuberculosis
4. Declarations
Consent for publication: Written informed consent for the publication of clinical details was obtained from the patient. A copy of the consent form is available for review by the editor of the journal.
Availability of data and materials: Not applicable
Competing interests: The authors declare that they have no competing interests.
Financial support and Disclosure: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ contributions: SPC & EPB coordination and design of the work; JHCF & MFCR analysis and writing; EV conception and coordination.
Authors information: Not applicable.
References:
- Wolfrum A, Kümmel S, Theuerkauf I. et al: Granulomatous Mastitis: A Therapeutic and Diagnostic Challenge. Breast Care 2018;13:413-418. doi: 10.1159/000495146
- Moule MG, Cirillo JD. Mycobacterium tuberculosis Dissemination Plays a Critical Role in Pathogenesis. Front Cell Infect Microbiol. 2020 Feb 25;10:65. doi: 10.3389/fcimb.2020.00065. PMID: 32161724; PMCID: PMC7053427.
- Sagara Y, Hatakeyama S, Kumabe A. et al. Breast tuberculosis presenting with intractable mastitis: a case report. J Med Case Rep. 2021 Mar 4;15(1):101. doi: 10.1186/s13256-021-02712-w. PMID: 33658078; PMCID: PMC7931525
- Baykan A, Sayiner H, Inan I. et al. Primary breast tuberculosis: imaging findings of a rare disease. Insights Imaging 12, 19 (2021). https://doi.org/10.1186/s13244-021-00961-3
- Global tuberculosis report 2022. Geneva: World Health Organization; 2022. licence: cc bY-Nc-sa 3.0 iGo.
- Tauro LF, Martis JS, George C. et al. Tuberculous mastitis presenting as breast abscess. Oman Medical Journal 2011, 26:53-55
- Strazzanti A, Trovato C, Gangi S. et al. Breast tuberculosis cases rising in Sicily. Int J Surg Case Rep. 2018;53:9-12. doi: 10.1016/j.ijscr.2018.09.048. Epub 2018 Oct 8. PMID: 30366176; PMCID: PMC6205060
- Jiménez M, Melero A, Sánchez R. Mastitis Granulomatosa. Clínica de investigación en ginecología y obstetricia. 2015;42(3):141-144. doi:10.1016/j.gine.2014.02.001
- Uçan ES, Alpaydın AÖ, Gündüz Karayazı D. et al. Tuberculous mastitis: A masquerading face of granulomatous mastitis. Tuberk Toraks. 2022 Sep;70(3):271-278. English. doi: 10.5578/tt.20229706. PMID: 36164951.
- Jyoti S, Amita Gupta. Tuberculosis in Pregnant and Postpartum Women: Epidemiology, Management, and Research Gaps, Clinical Infectious Diseases, Volume 55, Issue 11, 1 December 2012, Pages 1532–1549, https://doi.org/10.1093/cid/cis732






